TULSA, Okla. — More than 100 million Americans have been diagnosed with COVID-19, but experts say it’s likely twice as many have been infected. Some have had it more than once, and while many bounce back, countless others suffer unexplained symptoms for months or even years.
FOX23 Morning Anchor Michelle Linn looked into “long COVID-19″—what it can cause, who it can happen to and and how doctors are trying to understand a new condition.
Thousands of people suffer from long-haul COVID-19 symptoms, ranging from respiratory, to cardiovascular and neurological issues.
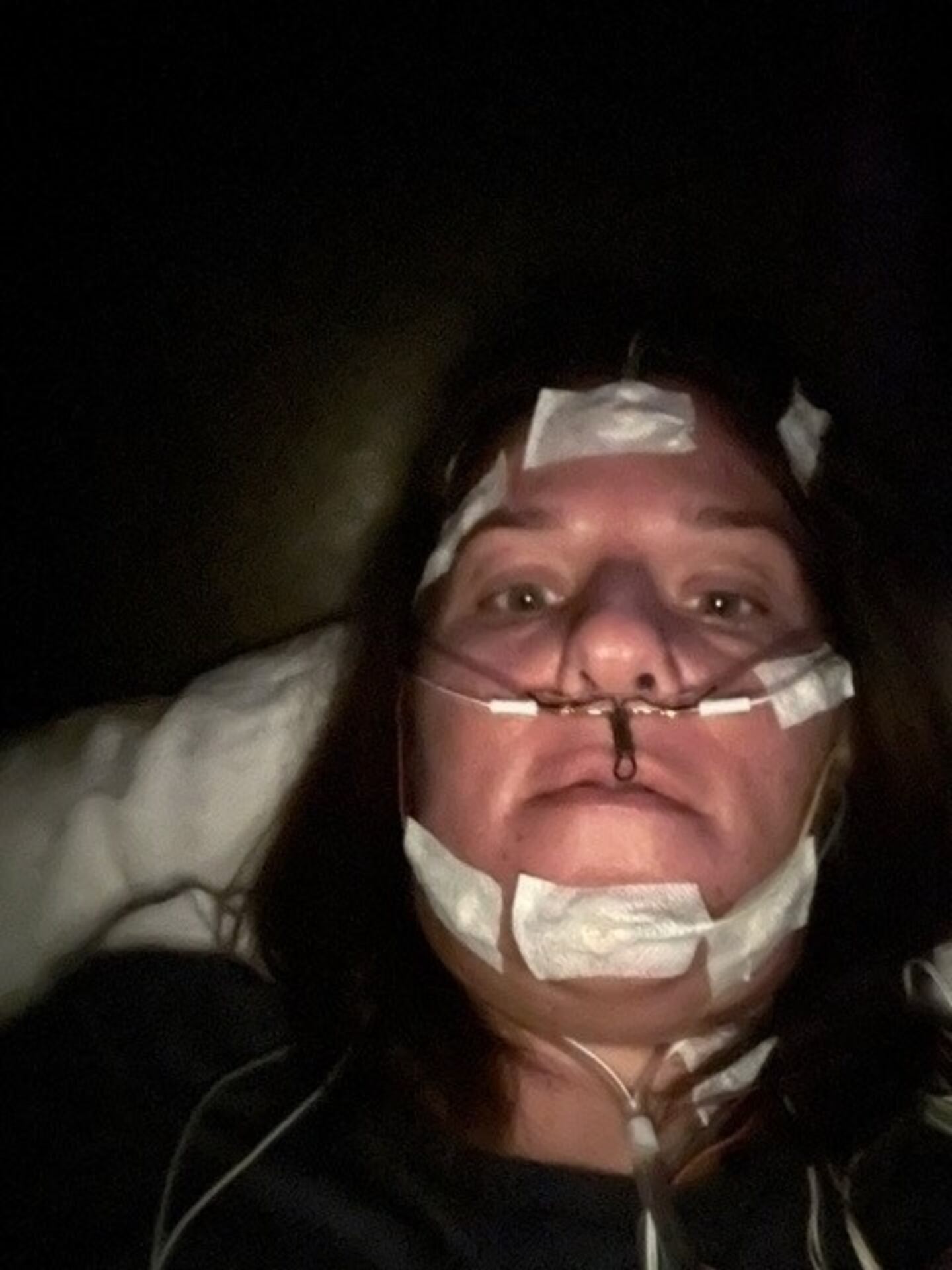
Amanda Finley said before she got COVID-19 in March 2020, she was an archaeologist. She said about three days in, she didn’t leave her bed and realized she needed help.
Her COVID-19 turned into pneumonia.
“They sent me home. I closed the door and I didn’t open it for four months. I didn’t want to get my neighbors sick,” said Finley.
Unable to work, she lost her home and wound up living in a tent. Finally, in May, she was able to secure an apartment in Kansas City, but she’s still struggling.
“I have a lot of cardiac issues now. I’ve been a regular in the ER lately with really elevated blood pressures, chest pain, shortness of breath,” Finley said. “‘Fatigue’ isn’t a strong enough word to describe this almost paralyzing feeling of you just can’t get up to do anything.”
Long COVID-19 can involve damage to the heart or lungs. Cardiovascular complications can include blood clots or stroke, even in younger patients. It can also involve vague symptoms, and it’s a challenge for doctors.
Brian Hurley described how his late wife’s doctor struggled to find what his wife was suffering from.
“He was just sitting there scratching his head, and he goes ‘You have something, but I don’t have a test to find it,’” said Hurley. “She had severe muscle pain, severe nerve pain.”
On Aug. 27, Hurley’s 38-year-old wife, and high school sweetheart, took her own life.
“Over time, she struggled with severe fatigue, brain fog, what they call neurocardiogenic sycophy, which is her brain and her heart weren’t talking,” said Hurley.
Patients who were never hospitalized with COVID-19 may now experience fatigue, brain fog, migraine headaches, muscle and joint pain.
Hurley said they started noticing his wife would have dizzy spells or she would fall over in the shower. It was getting worse to the point where she couldn’t work.
“The doctors were like ‘You just need more cardio. You’re just out of shape,’” said Hurley. “In her mind, aside from everything she had been through, the gaslighting of the medical community, the daily struggle, in her mind this was terminal anyway because it was getting worse ... That sounds morbid, but when somebody is in severe debilitating pain every single day and you can’t do anything about it, that’s all you want to do.”
Dr. Jeffrey Galles is the chief medical officer at Utica Park Clinic and said they’ve moved away from a post-COVID-19 clinic.
“I think people have a lot of fear around what happens if this persists and never goes away,” said Galles. “When you look at CDC and what they tell you the definition of long COVID is, anyone who has symptoms lasting 60-90 days, that you can’t explain through other testing ... That’s kind of broad, so it makes it really a challenge for providers to tie a diagnosis of long COVID to a patient.”
Now they’re educating primary care practitioners to ask patients the right questions, beginning with ‘Have you ever had COVID-19?’
Galles said the people in the hospital with COVID-19 or the people who get really sick are more likely to have long COVID-19 than the people with mild symptoms. But that doesn’t mean people with mild symptoms don’t get long COVID-19, too.
“Younger people get it, older people get it, so it’s across the entire spectrum of care,” Galles said. “In pediatric populations, there’s been some cases where kids have developed paralysis, and that can happen abruptly weeks and months after having COVID, and all of a sudden they can’t walk or can’t move arms or legs.”
“What we’ve found is some of these are autoimmune disorders where the nervous system is being attacked by the antibodies that are created from their COVID infection, so those are very bizarre and very unusual but they do happen,” said Galles.
He said it’s important for doctors to really listen and address patients’ concerns, and it’s important for patients to have hope.
“Most people who have long COVID are back to normal and functioning normal after a year, and there’s a lot of tools to help them get that way as well,” said Galles. “COVID will help us understand how a lot of other autoimmune or immune related illnesses develop.”
Hurley said his wife went from being a healthy, active mother to suffering crippling pain with no answers and no hope. She left behind two young sons.
“Brooke’s not in pain anymore. Brooke’s not suffering, but there are millions that are,” said Hurley.
The COVID-19 Long Haulers Support Facebook group started a support line in memory of Brooke Hurley. Anyone dealing with long COVID-19 can call 1-844-BROOKE-0. The line is answered 24/7, and is not a crisis line, but a place to talk to others who personally understand long COVID-19 symptoms.
“Primary care providers need to be very knowledgeable about what long COVID is,” Galles said. “People need to be validated. They need to know what the problem was to begin with.”
Galles said it’s really challenging for doctors because there is no test for long COVID. Instead they have to test for everything else that could be causing symptoms and eliminate things one by one. That’s why he said it’s so important, if you have head congestion, a sore throat, or chest congestion, to not brush it off, even if it’s relatively mild.
Taking a COVID-19 test will help doctors link any long-term symptoms to COVID-19.
According to the U.S. Census Pulse Survey, nearly 35 percent of people in Oklahoma who responded said they had COVID-19 symptoms that lasted longer than three months. Only Wyoming, Montana and Mississippi had a higher percentage of long COVID-19 symptoms than Oklahoma.
©2023 Imagicomm Tulsa, Inc.